
12.06.2025
The health checks all people with diabetes need to do
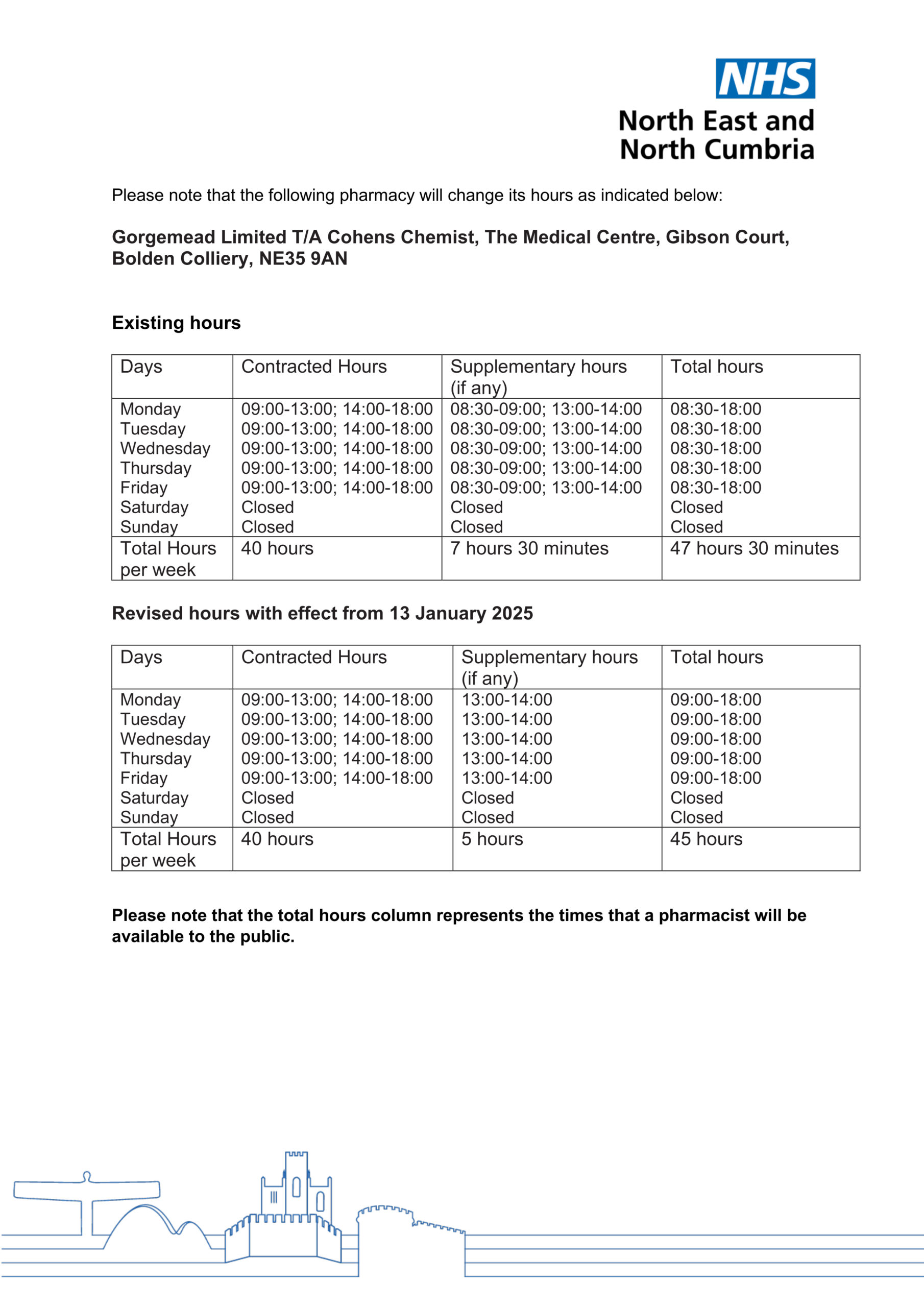
The full new opening hours are:
Monday – 9am to 6pm
Tuesday – 9am to 6pm
Wednesday – 9am to 6pm
Thursday – 9am to 6pm
Friday – 9am to 6pm
Saturday – CLOSED
Sunday – CLOSED
It is still open five hours in addition to its contracted hours, from 1pm to 2pm each weekday.
On Wednesday January 15, it will be at Hebburn Central from 9am to 3pm.
Healthcare professionals will be on hand to offer advice and support to people on a range of lung-related health conditions.
The event aims to bring in the expertise of South Tyneside and Sunderland NHS Foundation Trust’s assessment of breathing clinic (ABC) and acute respiratory assessment service (ARAS).
The Melissa Bus – Mobile Educational Learning Improving Simulation Safety Activities – is a double decker bus that has been designed to deliver healthcare education and training across the North East and North Cumbria.
It calls in at town centres and community centres to provide a ‘pop-in’ service for local people who may need help and advice on medical issues.
There is no need to make an appointment.
During its visit to Hebburn, it will also welcome the local Breathe Well Group Association, Talking Therapies and First Contact Clinical, which is a community interest company based in the borough and supports people with their health and wellbeing.
An NHS spokesman said: “The Melissa Bus is aimed at making it easier for people to seek advice on medical issues and we look forward to people in Hebburn calling in next week.”
These are medicines which can help with epilepsy, bipolar disorder and migraines (topiramate only).
NHS North East and North Cumbria would like to understand:
This survey is for people who live in North East England or North Cumbria. NENCICB would like to hear your views if you are:
Share your experience of talking about these medicines if:
Participants can complete as much or as little of the survey as they wish. If you choose to answer all questions, it will take approximately 15 minutes. The survey is anonymous, and no names are requested. It will remain open until February 28.
If you’re taking valproate, there is a risk of pregnancy, either by becoming pregnant yourself or by fathering a child.
Similarly, if you’re taking topiramate, pregnancy is a potential risk. These medications can be harmful if taken during pregnancy.
These medicines can harm a developing baby, leading to physical or learning disabilities, or both. It is crucial to use highly effective contraception while taking these medications, such as using two forms of birth control, to reduce the risk.
There are several people you can consult for advice about your medication, including your pharmacist, GP, doctor or nurse.
If you have any questions or need further help to complete the survey, please contact Jo Whaley, Involvement Lead, NHS North East and North Cumbria, at necsu.icb.involvement@nhs.net or or 0191 2172806.
Please complete the survey here or scan the QR code below.

Under the upgraded services, patients could receive their diagnosis weeks earlier with NHS chiefs vowing to boost patient experience and end the cycle of people getting stuck waiting between GP referrals and hospital appointments.
As part of the Elective Reform Plan, millions of people will receive quicker diagnosis and treatment to deliver routine care to nine in ten patients within 18 weeks.
The ambitious new blueprint will see more patients receiving a same day service – with a follow up consultation on the same day as their diagnostic test or scan.
Under the reforms, thousands more patients will receive a diagnosis and treatment date within a single day, providing people with peace of mind or a clear way forward for their treatment.
Acceleration of diagnosis times for patients will also come alongside a major expansion of ring-fenced elective capacity in both hospitals and the community – allowing routine care to be protected from winter pressures and future pandemics.
The plan for patients will also ensure that people are as fit and prepared as possible for treatment while they wait for an operation – this will not only boost post op outcomes and speed up recovery, but also reduce the number of on the day cancellations.
Patients waiting for surgery will be offered support to lose weight and stop smoking while they wait, with evidence showing that quitting tobacco four weeks before surgery can substantially reduce the risk of respiratory and wound healing complications by up to a third.
NHS Chief Executive, Amanda Pritchard, said: “While there are too many people waiting unacceptably long for care, NHS staff have made huge progress in bringing down long waits since the pandemic. And backed by government investment, alongside our commitment to continue to reform and innovate, we know that staff can significantly reduce waiting times across the country again.
“With 1 in 9 people in England on a waiting list, we know that there is more we can do to support those who are waiting for crucial tests and procedures.
“By making it easier for people to get timely access to the tests they need alongside direct referrals and same day checks and consultations – this plan will help thousands more people to get a faster diagnosis and quicker treatment or the all clear, so people can get back to living their lives as soon as possible, with peace of mind that they won’t need further treatment.
“The reforms set out in this plan are focused on improving how people access and experience routine care, as much as they are about waiting times – we are determined not to hit the target but miss the point. Simply put, this is a plan with patients at its heart.”
Secretary of State, Wes Streeting, said: “As patients, we’ve all experienced the hoops you have to jump through to get the test or scan you and your GP know you need. It’s a waste of patients’ time, delays diagnoses when every minute matters, and means consultants are forced to tick boxes rather than treat patients.
“The reforms we’re announcing next week will speed up diagnoses and free up NHS staff to treat more patients. Our plan for change will cut waiting lists from a maximum of 18 months to 18 weeks by the end of this Parliament.”
At the heart of the plan is a new gold standard retail offer with compulsory ‘customer service’ training for non-clinical frontline staff like receptionists, and all acute hospitals must have a named patients’ experience champion so those on the waiting list are kept fully up to date and supported with any wait for care.
It comes after hardworking NHS staff have already radically slashed the number of long-waiters since the pandemic, with the number waiting more than a year down by almost half since March 2021.
Healthwatch England Chief Executive Louise Ansari said: “We welcome this new plan’s focus on better waiting experiences, and not just wait times. In our own ‘Patient Vision 2030’ plan last year we had called for a focus on better trained admin staff and expansion of the NHS App, to ensure people got regular and informed updates on when they’d be seen, signposting to local support, and help to manage their condition while they waited for treatment.
“Overall, hospitals must tackle waiting lists in an equitable way – this relies on the NHS knowing who waits the longest, whether children, disabled people or those on low incomes, and taking action to address these inequalities.
“We now hope the urgency on tackling elective waits is extended to other areas such as mental health or GP appointments, within the upcoming 10-year health plan.”
Jacob Lant, Chief Executive of National Voices, said: “Tackling waiting lists is an obvious priority for both patients and the wider public, but with this announcement the government is also making it clear that the overall experience of waiting, and the ability to make meaningful choices about our care is just as important. By getting this right, the NHS can put an end to people feeling lost on lists.
“At the heart of this, we must see the plan deliver routine public scrutiny of who is waiting longer than they should. Current research shows that women, Disabled people and people from ethnic minority backgrounds all wait longer for care, as do people living on lower incomes. The NHS needs to pay specific attention to fixing the equity gap if key commitments around improving healthy life expectancy are to be met.”
President of the Royal College of Obstetricians and Gynaecologists, Dr Ranee Thakar, said: “We are encouraged to see the government’s commitment to improving elective performance, and welcome the ambitious targets set out in this plan. We are all too aware of the impact that the wait for elective care is having on thousands of women in the UK, leaving them living in pain and distress.
“We look forward to the implementation of this plan alongside wider measures we hope to see in the NHS 10-year-plan which we hope will ensure equity of care for all women. This includes ensuring the women’s health workforce across the system has the right support, time and funding to deliver the best care possible, and the widespread establishment of women’s health hubs across the country with the ongoing committed funding to maintain them.”
Adam Brimelow, Director of Communications at NHS Providers, said: “NHS trust leaders are doing everything they can so that patients are seen as quickly as possible. Nobody in the NHS wants people to wait any longer than needed for vital checks, scans, and treatment.
“Health leaders and their teams face huge challenges, but with the backing of this ambitious plan, they’re determined to reduce delays while tackling health inequalities and empowering patients.”
There were 4,102 patients in hospital with flu on Christmas Day, rising sharply by almost a quarter to 5,074 by Sunday 29 December. The new figures mean flu cases in hospital have quadrupled in a month (1,190 on 29 Nov).
There are warnings of continued pressure going into 2025, with amber cold health alerts for England issued by UKHSA as temperatures in the coming days are set to drop below freezing.
Hospitals are still experiencing pressure from a range of viruses, with an average of 723 patients with norovirus in hospital in the week ending 22 Dec, and 528 patients each day last week – although this has come down, it remains 40% higher than 378 the same week last year.
There was also an average of 74 children with RSV in hospital every day last week, up almost half on 50 for the same period in 2023, as well as an average of 1,184 beds occupied by patients with Covid.
The latest figures follow a warning by the NHS three weeks ago about low flu vaccine take-up rates that are still not at the levels we need to prevent further rises in admissions. Vaccine uptake currently stands at 37% for those in a clinical risk group.
While the national vaccination booking system has now closed, those eligible can still get protected by visiting a COVID-19 walk-in vaccination site or finding a pharmacy offering the flu vaccine.
Ahead of winter the NHS put in place measures to manage extra demand including upgraded 24 hour co-ordination centres, support for frequent users of A&E services, strengthening same day emergency care and providing more care in the community.
To prepare for an expected rise in winter pressure, the NHS had 1,301 more beds open last week than the same period last year (101,309 vs 100,008). There was an average of 648 more beds occupied each day compared to last year (90,200 vs 89,552).
Ahead of Christmas, NHS staff went above and beyond to discharge as many patients as possible who no longer needed to be there with 15,094 patients discharged on Christmas Eve, up more than 40% on the 10,495 discharges on average for the week before.
Further figures show the pressure on urgent and emergency services with a total of 98,118 ambulance handovers to hospitals last week, and 465,442 calls received by NHS 111.
Professor Julian Redhead, NHS national clinical director for urgent and emergency care, said: “These latest figures show the pressure from flu was nowhere near letting up before we headed into the New Year, skyrocketing to over 5,000 cases a day in hospital as of the end of last week and rising at a very concerning rate.
“On top of flu there is also continual pressure from Covid, while RSV and norovirus hospital cases are also higher than last year, with hospitals putting in place an extra 1,300 beds last week than the same time last year in expectation of this continued pressure from viruses and other demand.
“With what looks like an extreme cold snap expected right across England ahead of the weekend, we know the low temperatures can be dangerous for those who are vulnerable or have respiratory conditions so if you are at risk, do try and keep warm and make sure you are stocked up on any regular medication.
“Please continue to use NHS 111 and 111 online if you need advice and support for health conditions, and only use 999 or attend A&E in life-threatening emergencies.”
Secretary of State for Health, Wes Streeting said: “The tidal wave of flu this winter has seen more than three times as many patients in hospital compared with last year, putting huge pressures on the NHS.
“This government has ended the strikes so staff are on the frontline this winter rather than the picket line, introduced the new RSV vaccine, and put immediate extra investment into the NHS.
“But we have been honest from day one that the status quo isn’t good enough. We are investing in and reforming our NHS, and grasping the nettle of social care reform, to finally break out of the cycle of annual winter crises, because there is no solution to the crisis in the NHS that doesn’t involve a solution to the social care crisis.”
Dr Neil O’Brien, chief medical officer at North East and North Cumbria Integrated Care Board (ICB), said: “Ambulance and A&E teams are under real pressure and are focusing on the patients who need their help the most. Our thanks go to all our staff who are working incredibly hard to ensure patients get the care they need.
“If you’re seriously unwell over the next few days, it’s important that you get help. For anything else, please contact a community pharmacy, 111 online or by phone, an urgent treatment centre or your GP practice when it is open. Patients who come to A&E with minor problems should expect a long wait and may be asked to use a different service.
“We have planned carefully for a busy winter – including special respiratory hubs and Hospital at Home services so more patients can get the care they need without being admitted to hospital. You can really help by using NHS services carefully.”
Claire Jobling, head of operations north for the North East Ambulance Service, said: “We are experiencing additional demand on our service over the holiday period, especially on days when other healthcare providers operate on reduced hours or are closed.
“We are seeing pressure across the whole system, so we are asking that patients only call 999 in a life-threatening emergency. If it’s not a life-threatening emergency, please use 111 online for medical support with illnesses and injuries.
“By doing this, you are supporting the wider NHS and our service to ensure that we have enough resources to care for the poorliest patients at our busiest time of the year.”
For less urgent needs, patients can get help from NHS 111 online, which includes a symptom checker and will re-direct you to a health professional if you need medical attention. You can also phone 111.
Self-care advice is available online at www.nhs.uk, which also includes details of local pharmacy services.
Anyone needing urgent mental health support can get help by calling 111.
Families can also download the Healthier Together app for advice on common childhood illnesses and when to get medical help. Healthier Together is available from the App Store and Google Play.
Latest news
Quick online NHS services