
19.08.2025
Campaign urges parents against giving teenage children alcohol
These devices include pacemakers and implantable cardioverter defibrillators.
The service was launched to assist patients with heart devices, ensuring they can access MRI scans closer to home.
Based at South Tyneside District Hospital, the new service welcomed its first patients this summer.
Previously, patients faced long waits for appointments at the Freeman Hospital in Newcastle or were required to undergo alternative tests.
Now, they can receive their scans closer to home and with significantly reduced waiting times, which is crucial when awaiting a diagnosis.
The service was established through a collaboration among cardiology consultants, cardiac physiologists, and the MRI team at the Trust. They have created a safe referral and examination session, which has already welcomed over a dozen patients, with additional clinics scheduled.

Consultant Alykhan Bandali and MRI Lead Radiologist Miles Weston, front, with Chief Physiologists Eloise Shearer and Anthony Williams and Senior MRI Radiographer Laura Langley.
MRI scanners utilise powerful magnetic and radiofrequency fields to generate detailed images of the body’s interior, which can impact electronic and metallic implants. To ensure the safety of patients with Cardiac Implanted Electronic Devices, cardiac physiologists are available to monitor and support them throughout the MRI process.
Approximately 2,500 patients within the Trust have a Cardiac Implanted Electronic Device, and the MRI sessions are available to all those referred from across the region. Currently, all referrals to the team are processed within the Trust.
The STS Charity, which supports the Trust’s services, staff, and extras for patients, has contributed to the project by agreeing to fund specialised equipment necessary for the sessions.
Consultant Cardiologist Alykhan Bandali is among the dedicated staff members leading these sessions. He has previously played a key role in establishing a cardiovascular MRI service for the Trust. These scans not only aid in diagnosing various conditions, including certain cancers, but also help monitor heart function.
Dr Bandali said: “There are times when an MRI is just what we need to gather the information to make that step forward in someone’s care.
“The number of patients who have CIEDs is growing, and these devices are helping people live longer. Meanwhile, we know demand also rising for MRIs to help us diagnose an illness or monitor their condition.
“This is especially pressing when it comes to carrying out checks to find out if a patient has cancer, because the sooner treatment starts, the better.
“MRI is also an invaluable tool in the investigation or a wide range of other issues including musculoskeletal and neurological and when investigating the abdomen and pelvic areas.
“Having that scan closer to home is especially welcome when someone isn’t feeling well or for our older patients and their loved ones. These MRIs are a great addition to the service we offer, and I’m delighted our teams are working together to make it possible.”
More details about the work of the Trust’s Cardiology Team can be found through its Cardiology page, while information about its Radiology Department is available via its page.

©Paparazzi VIP Photography – www.paparazzivip.com – info@paparazzivip.com
Fran Davies, Past Master for Worshipful Company of Nurses, with STSFT Practice Education Team members Kelsey Dunning, Rachel O’Connor, Julie Manampan, Adam Remmer, Clare Adams-Graham, Barbara Goodfellow, Lesley Carlton, Eleanor Dungca, Laura Smith, Dawn Garrett, and Laura McGuire.
The team provides education for nurses, midwives and allied health professionals, as well as healthcare support workers and students.
The virtual reality work has created additional innovative learning environments for students. It has boosted the Trust’s capacity to offer student placements and offers a better training experience.
The Nursing Times judges said: “This project exemplifies the transformative power of technology in education and serves as a model for expanding clinical placements.”
Five other projects at the Trust are also due to find out if they are winners in awards which champion innovation.
It is also among three Trust teams shortlisted for the Bright Ideas in Health Awards, which is a regional celebration led by Health Innovation North East and North Cumbria.
It is in the Innovation in Clinical Education category at the ceremony, which will be held on Thursday, November 21.
Also shortlisted in the same awards is the Trust’s Speech and Language Therapy (SALT) Team, which is on the shortlist as Innovation Champion.
The SALT team is being recognised for its work to create a cookbook with head and neck cancer patients to help them recover and for hosting a social eating café and a stammering group for children. They have also launched an urgent clinic for ear, nose and throat (ENT) patients, they also developed training for others and lead the Mouthcare Team.
The team also works to reduce health inequalities, widening access to services including young people on the edge of care, and promotes continuous improvement through events, case studies, posters and podcasts.
Meanwhile, the Trust’s Assessment of Breathing Clinic is in the Innovation and Improvement in Reducing Healthcare Inequalities Award.
The Trust is also nominated for three titles in the national Smarter Working Live Awards 2024, which will also be held on the same evening.
Its Innovation Team is shortlisted in the Innovation as a Service Category for its work to support colleagues as they improve ways of working or come up with solutions to problems.
The Cancer Information Hub is in the Digital Inclusion Award section. The hub is an online resource for patients and their loved ones and offers videos and information about conditions, treatment, the journey they face following diagnosis, support available and more.
The creation of the Shoulder Reduction Bench is in the running in the Small-Scale, Big Impact section. The project was led by Sunderland Royal Hospital A&E consultants Ala Mohammed and Phil Dowson, who adapted a piece of gym kit to help treat people with dislocated shoulders quickly and without the need for sedation. The invention is now on sale to hospitals across the world.
Mark Taylor is the Trust’s Head of Innovation.
He said: “We are delighted to see our Practice Education Team collect the Nursing Times Award and excited to see they’re up for another award for their virtual reality work.
They’ve shown how technology can be used to help people develop their careers and build on their skills as they deliver care.
All of these teams shortlisted have used innovation to drive improvements, work in a better way or give our patients a better experience, sometimes all three.
I want to thank all those who have supported these teams and projects.
I’m very proud of my own team after it was shortlisted. We’ve been working hard to support innovators within our Trust over the last three years.
It has seen us help support innovators, protect their intellectual property and support their projects, as well as a lot of work behind the scenes which has all had a positive impact on our Trust.
We’ve also been helping to secure funding, have launched our own grant scheme and been busy working alongside partners to bring in their expertise.
All of these help bring on more projects to help our colleagues and those we care for.”
More information about the Trust’s innovation work can be found through the Innovation section of its website.
The research highlights a troubling trend as the likelihood of starting to smoke rises annually until age 25.
This comes as the Government faces increasing pressure to establish a ‘Smokefree Generation’ by raising the legal age for tobacco sales by one year annually, aiming to eliminate the death and disease associated with smoking.
In the North East, a survey reveals that over 77% of smokers regret ever starting, with 46% expressing a strong desire to quit.
Ailsa Rutter OBE, Director of Fresh and Balance, said: “Tobacco smoking is one of the biggest causes of disease, disability and death. No one who starts smoking ever means to smoke for life, but two out of every three smokers who do not manage to quit will die from their smoking.
Most people who start smoking start as children or young people. They underestimate the risks of disease, never expecting it to become an expensive and lethal addiction.
Most smokers in the North East want to stop and most would never risk starting to smoke or trying a cigarette if they had the choice again. The risks of smoking are also worse for people who started young.”
Earlier this month, smoking survivors and campaigners from the North East gathered in Parliament to urge the new Government to promptly commit to creating a smokefree generation. This plea comes over a year after the previous Government announced plans to raise the legal age for tobacco sales.
One of the attendees was Cathy Hunt, 58, a mum of four from County Durham. She was diagnosed with lung cancer and had half a lung removed in 2015 just two days before her 50th birthday. She underwent surgery again in 2022 when the cancer returned, and in June 2023 had a kidney removed due to cancer.
She said, “I started smoking when I was only 11 years old. Obviously, at the age of 11, I was not aware when I took that first draw of a cigarette how addictive and harmful smoking is.
At the age of 49, just days before my 50th birthday – my world was turned upside down. I was given the news I had lung cancer. Telling your children, that you have cancer from smoking is the worst conversation a person can ever have, watching the fear and uncertainty wash over them and knowing you have changed their world forever.
I am begging the Government and MPs to commit to a smokefree generation and raise the age of sale. Too many people are becoming ill and dying from smoking. We now have a chance to stop the start.”
There is strong North East support to create a smokefree generation with:
(YouGov)
The North East has a unique declaration for a smokefree future with a clear vision: “A smokefree future, free of the death and disease from tobacco, is needed, wanted and workable”. This would improve the health and wealth of our region’s most disadvantaged communities more than any other measure.
For support around stopping smoking, talk to your free local stop smoking service or your doctor.
For top tips to stop smoking for good, click here.
To boost cervical screening rates, this initiative aims to empower and educate women and individuals with a cervix about the vital importance of smear tests.
The first of three workshops will take place at the Comfrey Project in Gateshead on Wednesday November 20 at 10.30am.
Participants will receive £25 per hour for their involvement, paid via bank transfer from Northumbria University or by Love2Shop vouchers.
According to reports, almost all (99.8%) of cervical cancers are preventable if eligible individuals engage with the NHS Cervical Screening Programme. However, in the North East region, around 38,000 people aged 24-64 are not up to date with screening.
Cervical screening is one of the most effective ways to protect yourself from cervical cancer. Despite its importance, one in three women under 35 do not participate in routine screenings.
It is not a test for cancer, it is a test to help prevent cancer.
Cervical screening is a trusted method for detecting abnormalities that could lead to cancer. It also tests for Human Papillomavirus (HPV), helping to prevent cervical cells from becoming abnormal.
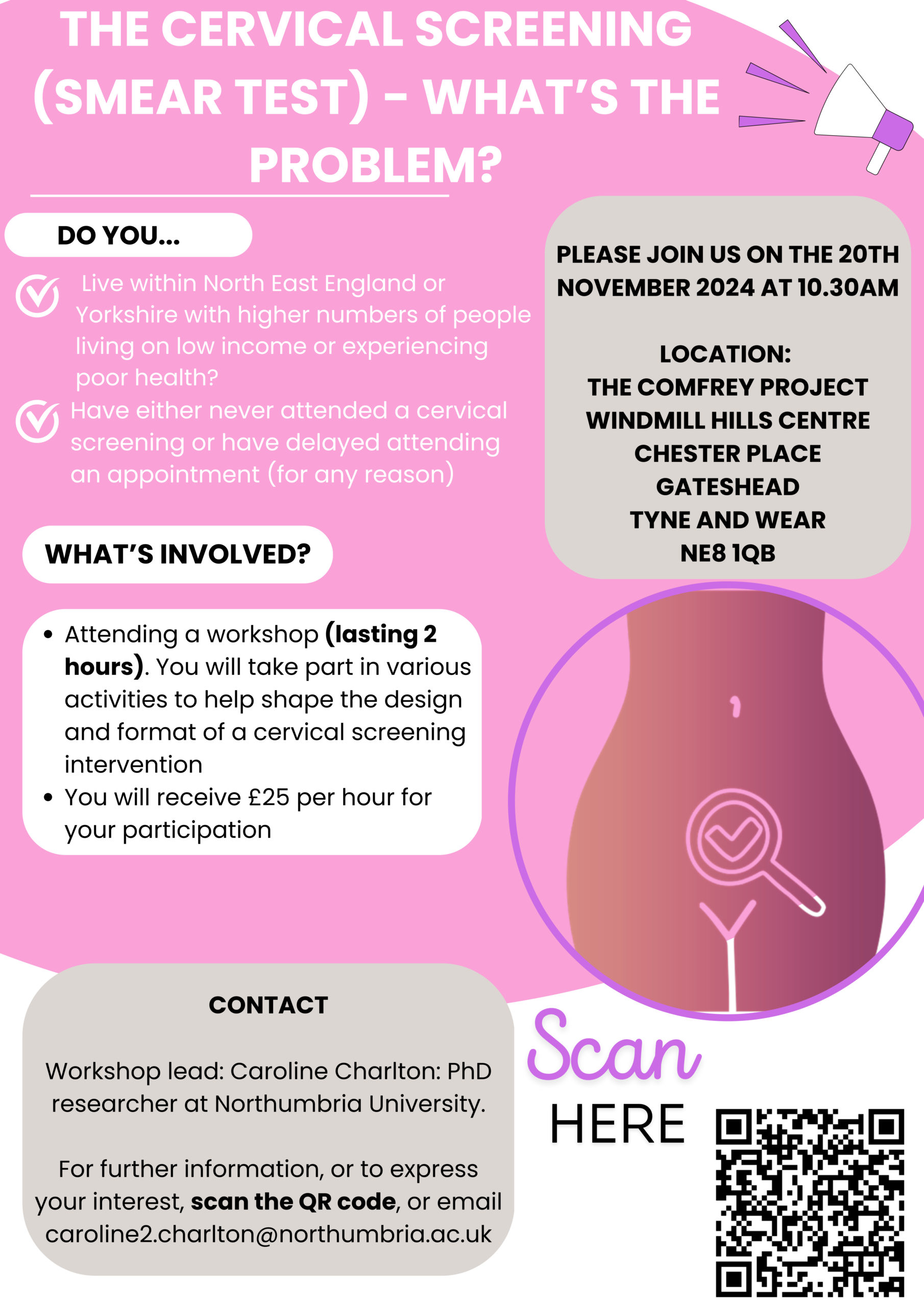
To discover more and share your insights on cervical screening, join the initiative to raise awareness about the vital importance of smear tests – you can help make a difference.
For more information, scan the QR code or click the link below.
Register your interest here.
If you have any questions, please contact caroline2.charlton@northumbria.ac.uk.
The initiative stems from the actions outlined in the Ockenden Review regarding maternity care at Shrewsbury and Telford Hospital.
Annette, Ellie and Jan are advocates from ‘People First’ (an independent advocacy organisation) covering South Tyneside and Sunderland who will help anyone who has experienced an adverse outcome voice their concerns.
They do not work for the NHS or Social Services – meaning they can support people who are not happy with their care to have a say.
They will guide you through the process, ensuring your voice is heard and your concerns are addressed. Services are free and remain confidential.
You can seek advice from an advocate if:
 The North East and North Cumbria Information Commissioning Board is responsible for managing your personal information related to your interactions with the MNISA service. NHS England oversees the reporting system utilised by the MNISA service, ensuring secure storage of any information you provide.
The North East and North Cumbria Information Commissioning Board is responsible for managing your personal information related to your interactions with the MNISA service. NHS England oversees the reporting system utilised by the MNISA service, ensuring secure storage of any information you provide.
To work with Maternity and Neonatal Independent Senior Advocates, you need to have been looked after in the North East or North Cumbria area.
To better assist you and your family, the advocates would be pleased to arrange a meeting. They offer several options for discussion, including in-person meetings, phone consultations, and video calls.
They will accompany you to meetings, guide you through the maternity and neonatal healthcare system, assist you in understanding your care experience, and support you during investigations and complaint processes.
MNISA advocates are committed to providing professional support to you and your family, ensuring your voices are heard by maternity providers.
For more information, please download the guide or email MNISA@wearepeoplefirst.co.uk or call 0300 303 8037.
As part of the first shift, ‘from hospital to community’, the Government said it aims to establish new neighbourhood health centres that are closer to homes. These centres will allow patients to access a range of services including family doctors, district nurses, care workers, physiotherapists, health visitors, and mental health specialists – all in one location.
In transforming the NHS from analogue to digital, the Government will create a more modern NHS by bringing together a single patient record. New laws are set to be introduced to make NHS patient health records available across all NHS trusts, GP surgeries and ambulance services in England – speeding up patient care, reducing repeat medical tests, and minimising medication errors.
By moving from sickness to prevention, the Government wants to shorten the amount of time people spend in ill health and prevent illnesses before it happens. The Health Plan will explore the opportunities smart watches and other wearable tech may offer patients with diabetes or high blood pressure, so they can monitor their own health from the comfort of their own home.
Health and Social Care Secretary Wes Streeting said: “When I was diagnosed with kidney cancer, the NHS saved my life, as it has for so many people across our country. We all owe the NHS a debt of gratitude for a moment in our lives when it was there for us, when we needed it. Now we have a chance to repay that debt.”
The Government said it is vital it hears from patients, experts and the NHS workforce to revolutionise the way people access healthcare. Responses will shape the Health Plan to fix what it describes as a broken health service and deliver the Government’s mission to build an NHS fit for the future.
NHS England Chief Executive Amanda Pritchard said: “The Ten Year Health Plan is a chance to make the best practice, normal practice across the country. So, we will be carrying out the largest ever staff engagement exercise in NHS history and leaving no stone unturned as we seek to harness frontline views, alongside those of patients and the public, to ensure this happens.”
Rachel Power, Chief Executive of The Patients Association, said: “We warmly welcome this ambitious initiative to engage with patients, staff, and the public on the future of our NHS. For far too long, many patients have felt their voices weren’t fully heard in shaping health services. This national conversation, initiated by the Government, marks a significant step towards genuine patient partnership and puts patients at the heart of the NHS’s evolution.”
Louise Ansari, Chief Executive of Healthwatch England, added: “We urge everyone to have their say on how the NHS should deliver better care to people where and when it is needed, more support to help people stay well, and a culture of listening to and acting on the views of patients.
“All too often, people face unequal access to care, with disabled people and those on lower incomes being particularly at risk. The NHS belongs to us all, so you must speak up and help create a health service that is fit for the future – equal and inclusive for everyone.”
Latest news
Quick online NHS services