
19.07.2025
One year to go! Countdown begins for region’s new Eye Hospital
North East & North Cumbria Integrated Care Board (NENC ICB) asked Healthwatch through its work on the Living Well Alliance framework to gather insights into the mental health care experiences of older people.
NENC ICB specifically wanted to know if older people felt they experienced ageist attitudes and assumptions about their mental health which led to them being excluded from services and support that could help them to enjoy a healthier and happier later life.
Between May and September 2024, our engagement team spoke to 123 patients aged 65+ in 12 healthcare settings, asking them the following question provided by NENC ICB: “When you meet professionals in health and social care, do they ask about your mental health?”
Our key findings included:
Of the participants, 66% were female, and 99% were white British. Through our conversations across various groups, there were several clear themes.
Participants highlighted that time constraints during doctor’s appointments often discouraged them from seeking help for their mental health. One said: “You are told that you only have so long with the GP, they don’t have the time, and I wouldn’t ask for two separate things.”
Many expressed that using e-consult services can be particularly challenging. A significant number of participants said they do not own a mobile phone or use a computer, making technology a barrier for some.
Throughout discussions the word stigma was used, although participants acknowledged that mental health is more widely discussed today. One said: “It’s embarrassing to talk about your mental health, I would like them to initiate the conversation.”
Participants told us that re-phrasing the term ‘mental health’ would go some way to removing the stigma attached.
Perceptions identified within several groups were that as you get older the doctors “don’t care”, and many health issues are put down to your age. One participant described the experience of talking to a doctor as feeling like “talking to a brick wall”, citing a lack of eye contact as doctors focus on their computers.
Many expressed frustration at rarely seeing the same doctor twice, believing this harms the doctor-patient relationship.
We also received positive feedback, with a number of participants noting that younger doctors are seen as more attuned to mental health issues.
Many respondents acknowledged that their physical health affects their mental well-being. Several emphasised the importance of self-care, highlighting the value of regular check-ups, such as annual MOTs or well-women clinics, in taking personal responsibility for their health.
Participants shared various strategies for supporting their mental health, including healthy eating, regular exercise, and combating social isolation by joining local voluntary groups to build friendships.
One said: “I attend a Happy at Home group, it gets me out of the house and some members of the group come and visit me at home, so I don’t feel lonely or isolated.”
Responding to our findings, the NENC ICB said: “The insights within the report will be utilised to shape how we transform services to ensure that our older residents receive holistic equitable care.
“Furthermore, we intend on developing an age-friendly health system with special features, structure, and functions to meet the special needs of older people and improving their health status and quality of life.
“We will continue to work collaboratively with Healthwatch to ensure that the findings of the engagement inform the next phase of addressing these important issues.”
Healthwatch would like to thank NENC ICB and all participants for their help in this research.
She dialled 999 and an ambulance rushed the 64-year-old to Sunderland Royal Hospital.
There, he was given medicine to get rid of blood clots on his brain, which is known as thrombolysis.
A stroke is when blood stops flowing to part of the brain. It affects speech and movement and needs urgent medical help in hospital because it can be life-threatening.
Following tests and scans, Martin was taken to the RVI in Newcastle in case he needed surgery. Thankfully, the team there found the drug treatment had worked and he was transferred back to Sunderland to recuperate.
After a night on E58, the hospital’s acute stroke ward, Martin was well enough to be discharged.
It meant he was able to make the marriage ceremony of his daughter Emily and her now husband Scott Phinn.
Emily, 27, works as an early learning practitioner, while Scott, 29, is a retail manager in the motor industry. They exchanged vows at Shotton Grange, in Seaton Burn, on Thursday, October 31.
Martin, who was born in Sunderland Royal Hospital and is originally from Whitburn, retired two years ago after 35 years of working off-shore.
He has shared his experiences after contacting South Tyneside and Sunderland NHS Foundation Trust (STSFT) with a note of thanks to the team who treated him. He also sent on photos to share of his family’s special day.
The North East Ambulance Service (NEAS), which helped get Martin the swift hospital care he needed, has also stressed how vital it is to act and get treatment quickly.
In his message to those who cared for him, he said: “The staff were amazing and this was so reassuring for me, as my daughter got married the next day.
“I never thought it was something that I may miss out on. Because of your team’s dedication, I was able to walk my daughter down the aisle, just a day after having my stroke.
“The day was amazing, so thank you all, you worked miracles for me.”
Martin, a keen photographer and videographer, managed to film the day’s events, while Hope Visual Productions captured the moment Martin was able to walk Emily down the aisle.

Martin said: “I was at home when the stroke began, after just finishing my usual morning press ups. I was totally unaware anything was wrong and thought my wife was massively overreacting by calling 999 for an ambulance.
“We had a very busy day ahead, as I had a mountain of video camera equipment to set up for the big day and thought I was fine. My wife however, noticed all the tell-tale signs straight away, and despite assurances from me that I was fine, wouldn’t listen and called 999.
“The ambulance arrived in record-breaking time and whisked me up to Sunderland with the blues and twos going. The team there rushed me through the system and gave me thrombolysis.
“After a good few more tests and scans, I was then rushed up to the RVI in case I needed surgery. After the tests at the RVI showed I had improved, and the clot-busting drug had worked, I was returned to Sunderland for overnight observation.
“The staff managed to get me all checked out, scanned and a suitable aftercare package sorted with new medication in order to get me to the wedding. The groom and best man even came to the hospital to make sure that I got there in time to walk my daughter down the aisle.”
Martin is continuing to recover at home, but has been keeping busy by editing video clips of the day.
Dr Richard Telford is Clinical Director of Rehabilitation and Elderly Medicine, which includes the stroke services run by STSFT.
He said: “We’re delighted to hear Martin is making a good recovery and we and the RVI were able to help him get to such a special occasion for his family. We wish the newlyweds every happiness.
“The swift actions of his wife undoubtedly helped the North East Ambulance Service our team and then those at the RVI get Martin the care and treatment he needed as quickly as possible.
“Strokes have three warning signs, weakness in the face, weakness in the arm or arms and speech problems, where someone might slur their words or sound confused.
“If this happens, it is so important to call 999 as soon as you can. As Martin’s family now know, every second counts.”
Dan Haworth, consultant paramedic for the North East Ambulance Service said: “Every year we respond to around 5,000 patients who are experiencing the symptoms of a stroke across the region. Of this 5,000, roughly 3,000 of these patients are then confirmed to be experiencing a stroke when they get to hospital.
“When someone makes a 999 call with a suspected stroke, getting help fast is critical. Everyone, from our emergency operations centre colleagues to our ambulance crews, are trained to be able to identify, triage, and manage strokes but making sure that call for help is made early can make a world of difference to a patient’s outcome.
“Martin’s story is a clear example of how making sure 999 is called quickly, can save lives. Thanks to the swift actions of his wife, we were able to get a crew to him quickly and help him begin his journey to recovery.
“We’re so glad to hear that Martin is now on the mend from what was, undoubtably, a very worrying time for him and his loved ones. We are even happier to hear that he was able to walk his daughter Emily down the aisle at her wedding.”
More details about strokes, their symptoms, treatment, recovery and causes can be found through the NHS’s Stroke information page.
Main image: Nikolaos Axelis/Hope Visual Productions.
Overlooked by Big Ben in the Queen Elizabeth II Centre, the event included keynote speaker Baroness Gillian Merron, Parliamentary Under-Secretary of State at the Department of Health and Social Care and Healthwatch sponsor.
Baroness Merron told those in attendance: “Thank you for all you do to seek out, amplify and champion the experiences of those who use our health and care services.”
Healthwatch England Chief Executive Louise Ansari said Healthwatch colleagues’ efforts to reduce health inequalities ‘day in, day out’ fills her with enormous pride, while Chair Professor David Croisdale-Appleby said he had been ‘stunned’ by the network’s achievements.

John added: “There was a great turnout from across the country and it was really interesting to chat to other delegates about the different ways that other Healthwatches are run. We also found the sessions which discussed the challenges and future of adult social care very useful.”
Feedback from South Tyneside residents has been included in a national report on dentistry by Healthwatch being published later this week. Read it here.
The operators and the areas they cover are:
The services offered can include domiciliary care, dementia support, respite care, live-in care, end-of-life care, practical support and companionship.
Healthwatch South Tyneside is currently contacting 200 users of home care services – 50 in each zone – on behalf of the borough council to conduct a survey over the phone or arrange its completion online or via post.
Questions range from timekeeping to the quality of care and treatment, time allocated to visits, how easy it is to contact the care agency and details of any issues experienced.
The next phase will see Healthwatch survey staff who deliver the home care services on behalf of the four firms, and ask them to give their feedback on their role and the support they receive to deliver it.
Staff are being asked to complete a short online survey which can be accessed here.
The survey for users of the home care service can be completed here. Please note – we only require feedback on the four named providers.
Healthwatch will analyse the survey findings and produce a report for South Tyneside Council with recommendations based on any common issues raised by service users.
Getting the right care, at the right time and in the right place is important for everyone. For children and young people, however, delays can have especially significant and lasting consequences. Some treatments and interventions are less effective if not administered at a specific age or developmental stage – and the opportunity to intervene can be missed completely if the wait for diagnosis is too long.
Many children and young people are not currently getting the support they need. This year’s State of Care report highlights this as a risk not just for today, but for the future. Children who do not receive the care they need today are at increased risk of becoming adults with long-term mental or physical illnesses, which could affect their quality of life and their ability to contribute to society tomorrow.
More broadly, timely access to good care continues to be a struggle for many, and inequalities in care persist. And issues getting access to services are often exacerbated by deprivation; in 2023/24, attendance rates for urgent and emergency care for people living in the most deprived areas of England were nearly double those for people in the least deprived areas.
Analysis conducted for CQC showed that for people attending for mental health reasons, the difference was over three times higher for those in the most deprived areas.
The safety and quality of some services is not good enough. CQC’s review of maternity services shows that women and babies are still not receiving the high-quality maternity care they deserve, and women from Black and ethnic minority backgrounds continue to be more at risk of experiencing poor maternity care and outcomes.
Mental health services are also a cause for serious concern. Lack of resources, ageing estates and poorly designed facilities are affecting the safety of inpatient wards. CQC’s special review of the care provided by Nottinghamshire Healthcare NHS Foundation Trust also identified wider concerns around community mental health services, leading to recommendations to improve oversight and treatment of people with serious mental health issues.
CQC has particular concerns about children and young people’s mental health services, where demand continues to rise. In 2023, 1 in 5 children and young people between the ages of 8 and 25 were estimated to have a mental health disorder. While the mental health workforce has grown, problems with staffing and skill mix remain. Across the country, services are facing challenges in recruiting staff including nurses, psychologists, occupational therapists, and consultant psychiatrists – all of which are having an impact on capacity, and therefore on the availability and regularity of appointments.
Mental health difficulties experienced as an adult often begin in childhood or young adulthood. Early intervention increases the prospects of good mental health in later life – but delayed or inadequate intervention decreases these chances.
CQC commissioned work to gain further insight into the experiences of children and young people when using mental health services. From this, one young person described the consequences of what they felt to be inadequate support from community services, leading to long-term hospitalisation:
“I didn’t know what to do because I didn’t have any GCSEs and I thought no one’s gonna want to give me a job and I’m not gonna be able to go to college…I wasn’t a normal person of my age because I was in hospital and I missed out on all the things”.
Conversely, a young person who had a positive experience reflected: “I do still think back on my time at CAMHS and I was like, if I didn’t [get that support], I would be in such a different place today… I got very lucky.”
Further research commissioned by CQC into attendances at urgent and emergency care settings by people with a mental health issue found that those aged 18 to 21 consistently have the highest rates of presentation for mental health issues at both emergency departments and urgent care centres. Not getting the right help at the right time can lead to people’s symptoms to deteriorate and they can then end up in crisis and/or inappropriate environments, such as urgent and emergency care.
CQC’s inspections of urgent and emergency care services found issues around triage and patient flow that affect care for all patients but identified specific issues around care for deteriorating children. Low numbers of children’s nurses and gaps in staff training in safeguarding and recognising sepsis meant that in some services, there was a risk that a deteriorating child might not be identified quickly, with patients at risk of sepsis not being assessed and treated promptly. Actively involving parents in their child’s care decisions and addressing their concerns promptly is critical to safety.
Last year’s State of Care warned about movement to a two-tier healthcare system – where those who can afford to pay for treatment do so and those who can’t face longer waits and reduced access. This remains a concern, starkly illustrated in dental care. CQC conducted a dental access survey of 1,000 people earlier this year, which found that people relied more on private care where NHS activity is lowest, and that access issues had a clear impact on children and young people.
Parents said they felt pressured to go private and found it difficult to get appointments, even in emergencies, and that children were left in pain while waiting for an emergency appointment. It is notable that the tooth extraction rate related to decay is nearly 3 and a half times higher for children and young people in the most deprived communities, compared with the most affluent.
The report also highlights concerns about care for autistic people and people with a learning disability – both the quality of care and access to it. The waiting time to begin assessment for a possible autism diagnosis is far too long, with average waiting times even longer for children and young people – 356 days in April 2024 compared with 238 days for adults. An autism diagnosis can be vital to getting the right help and support and can make a critical difference for children who are struggling at school.
In inspections of providers, CQC has seen examples where specialist services for children and families with complex needs were pivotal in leading multi-agency working and sharing learning. A limited review of integrated care system (ICS) plans, undertaken before the pause in CQC’s assessments of ICSs also saw some early positive signs, including transformation plans for children and young people’s services. Some ICSs have children and young people scrutiny boards to provide governance and monitor planned implementation.
Waiting times for services remain a problem within ICSs, and the main challenge is demand versus supply – a significant increase in requests at the same time as workforce shortages. There was variation between some published ICS plans or a lack of clarity about their intended outcomes. But some ICSs had examples of action already taken – for example, one described virtual wards that had supported more than 1,150 children.
However, a greater focus on children and young people’s services at both a national and local level is needed. This should include consistent funding targeted to areas of early intervention, better understanding by systems of the gaps in provision of care and treatment for their population to ensure that local areas can meet the needs of their children, improved management of demand and communication with children and their families.

Ian Dilks, Chair of CQC, said: “This year’s State of Care describes issues with access to and quality of care and the impact on people who use health and care services – with particular focus on the many children and young people who are not getting the care they need when they need it.
“While some children are receiving timely, appropriate care, we know that there are more who don’t, with potential long-term repercussions for their mental and physical health. Action now – targeted funding for early intervention, better understanding of local need and improved management of demand, and genuine two-way communication with children and families – will help to ensure a healthier population tomorrow.
“The health and wellbeing of a nation’s children has been described as the best predictor of its future prosperity; failing to ensure good, safe care for our children today also risks failing their future.”
James Bullion, Interim Chief Executive of CQC, added: “We have consistently highlighted the fragility of the adult social care sector – and the situation remains precarious.
“The number of new requests for local authority adult social care support that resulted in no service being provided has increased by over quarter over the last 5 years. And in April this year, waits for care home beds and home-based care accounted for almost half of delays in discharging patients who’d been in hospital for more than 14 days. Nearly 4,000 people are delayed on an average day – that’s 50 double-decker buses full.
“While vacancies in adult social care have dropped slightly, the average staff vacancy rate in social care is still nearly three times higher than in the national workforce – and care workers, despite the crucial job they do, remain among the lowest paid members of society.
‘Some providers are struggling to provide good, safe care – but there are also many outstanding adult social care providers who put the people they care for at the centre of their decision making, as the case studies included in this report demonstrate.”
Commenting on the report, Chris McCann, Healthwatch England’s Deputy Chief Executive said: “This report makes for disturbing reading and reflects what many people, especially parents and young people, are telling us about problems accessing care and the impact this can have.
“When it comes to dental care, these issues are particularly acute. Parents have told us that their school-aged children have never seen an NHS dentist due to a lack of available appointments. Some are told their child can only be treated under the NHS if the parent registers as a private patient. We have alerted NHS England, urging them to remind dentists that this is a breach of their contract.
“A child experiencing untreated dental problems cannot eat, sleep, or properly concentrate in class. Fundamental changes to NHS dentistry are needed urgently to improve access and prevent a new generation from living with poor oral health throughout their adulthood.
“The CQC findings also confirm experiences shared with us about other issues, such as the long waits for ADHD assessments. A problem which is highlighted by the story of one mother who sought help for her child in year three, but support didn’t start until his second year of secondary school.
“It is essential that the NHS does all it can to speed up access for patients and reduce the impact that long waits have on people’s mental and physical health.
“However, we also need long-term solutions. The government consultation on the NHS’s ten-year plan provides an opportunity to turn the corner on long waits for care. We’d urge everyone, especially parents and young people, to share their views and help shape the healthcare system for the future.”
Read the full report here.
Healthwatch England response : https://www.healthwatch.co.uk/response/2024-10-25/our-response-state-care-report
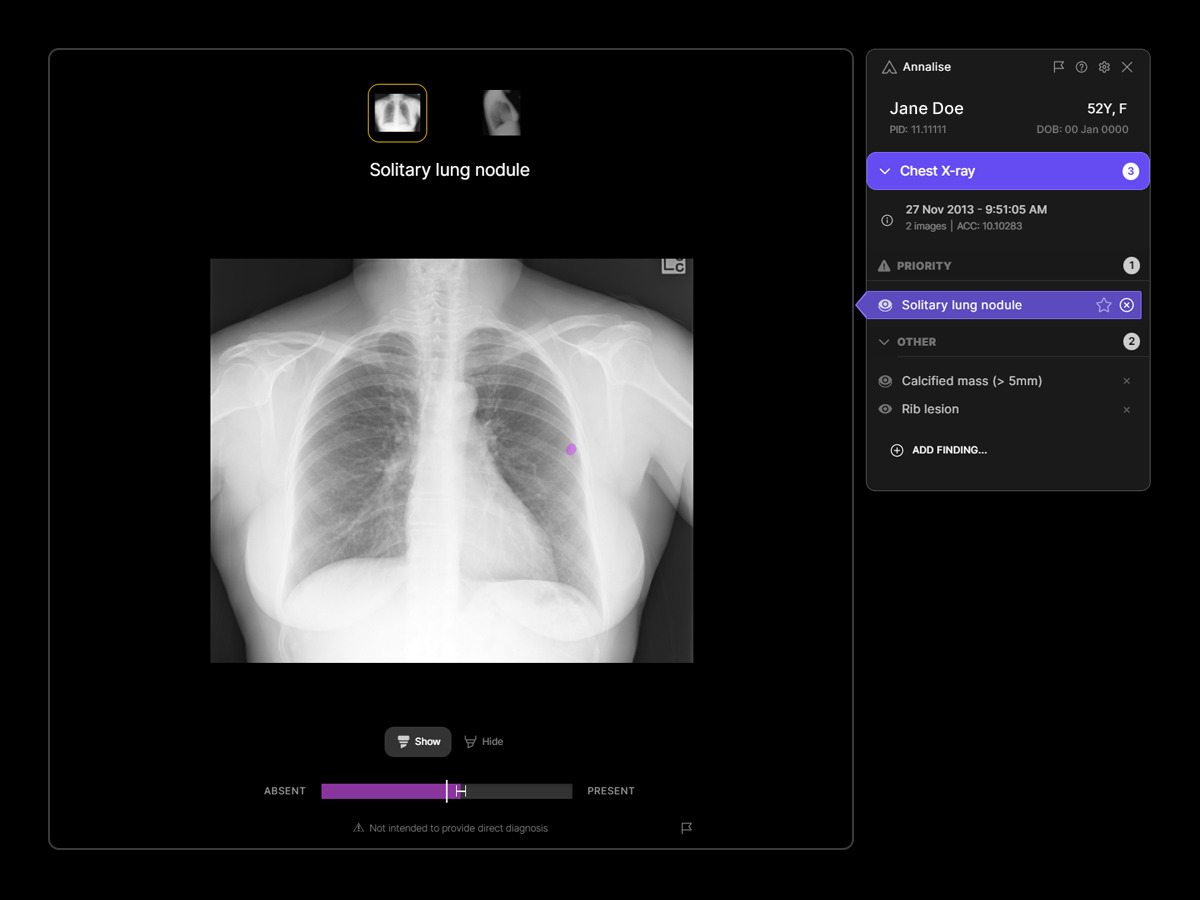
The AI technology serves as a vital second pair of eyes for clinicians, capable of prioritising cases where X-rays reveal suspicious findings that could indicate lung cancer. It has demonstrated a remarkable 45% improvement in diagnostic accuracy and a 12% boost in diagnostic efficiency.
The collaboration with Annalise.ai was made possible by a successful funding bid through the region’s Imaging Network, backed by the Provider Collaborative, which unites all NHS Foundation Trusts.
The bid gained support from the Northern Cancer Alliance and successfully secured funding from NHS England’s AI Diagnostic Fund (AIDF), which allocates £21m to provide 12 imaging networks across 65 NHS trusts in England.
Lung cancer is the leading cause of cancer death in the North East and North Cumbria.
It also has the highest incidence in England, with 117 people per every 100,000 developing the disease, compared to 88.5 people per 100,000 in London.
Six in 10 people will survive more than five years if lung cancer is diagnosed at the earlier stages, but this falls to just one in 10 for those diagnosed at the latest stage.
The disease has many causes, but a significant aspect is the higher smoking rates across generations in our region compared to the national average. The North East and North Cumbria are home to some of the most disadvantaged communities, where residents already contend with health inequalities.
The rollout of AI technology has the potential to save lives across the North East and North Cumbria, bringing hope to many individuals in their battle against cancer and strengthening our regional fight against the disease
Consultant Radiologist at South Tyneside and Sunderland NHS Foundation Trust, Dr Peter Hewitt said: “By using the AI tool, it will interpret chest X- rays within a minute of them being taken and it will put patients with suspected cancers at the top of the list for reporting.
“It will improve the accuracy and speed of reporting, acting as a second pair of eyes and will pick up anything subtle.”
Ken Bremner MBE, Chair of the North East and North Cumbria Provider Collaborative and Senior Responsible Officer for the region’s imaging network, is also Chief Executive of South Tyneside and Sunderland NHS Foundation Trust.
He said: “The arrival of this technology for the region’s NHS is a very welcome addition to our fight against lung cancer and the terrible impact it has on our region’s communities. By using the AI tool, we will be able to improve the time it takes for treatment to begin for anyone who receives a lung cancer diagnosis. It will help us to save people’s lives and, importantly, catch more cases quickly.
“The earlier we can start treatment for lung cancer the better – this will go some way to make that difficult time following a diagnosis easier for patients as they start their treatment journey.”
Latest news
Quick online NHS services